
Navigating postpartum sexual health can feel like a delicate dance. If you’re wondering how soon after childbirth can you have intercourse, this guide breaks it down with timelines, comfort tips, and real-world support. New motherhood brings joy, but it also comes with physical healing, hormonal shifts, and emotional adjustments. A common question many new parents ask is: when can I resume sex after childbirth? The answer varies for everyone. Therefore, this guide explores healing timelines, practical tips for comfort, and ways to reconnect with your partner at a pace that feels right. ❤️ To support your full recovery, including core strength and bladder control, don’t miss women’s pelvic health.
Take the 1-minute Postpartum Intimacy Check →Table of Contents
- Key Takeaways for Postpartum Intimacy
- How Soon After Birth to Resume Sex?
- OB/GYN Advice and Hormonal Impacts
- Managing Discomfort and Emotional Readiness
- Communicating with Your Partner
- When to Seek Professional Support
- Intimacy Readiness Checker
- Frequently Asked Questions About Postpartum Intimacy
- Conclusion
Key Takeaways for Postpartum Intimacy
- Many healthcare providers suggest waiting 4–6 weeks if you’re wondering when you can resume sex after childbirth, but consult your doctor for personalized advice.
- Physical recovery is vital, but emotional readiness matters just as much for postpartum intimacy. Hormones, fatigue, and new responsibilities can impact desire.
- Open communication with your partner fosters understanding and supports a gentle reconnection.
- Discomfort is common. Use lubrication, focus on pelvic floor health, and try comfortable positions. Seek help if pain persists.
- Always consult your OB/GYN for personalized advice on resuming sex after childbirth.
How Soon After Childbirth Can You Have Intercourse?
Your body undergoes remarkable changes during pregnancy and childbirth, impacting postpartum sexual health. Consequently, whether you had a vaginal delivery or a C-section, significant healing is necessary before you consider resuming sexual activity. Here’s what to expect.
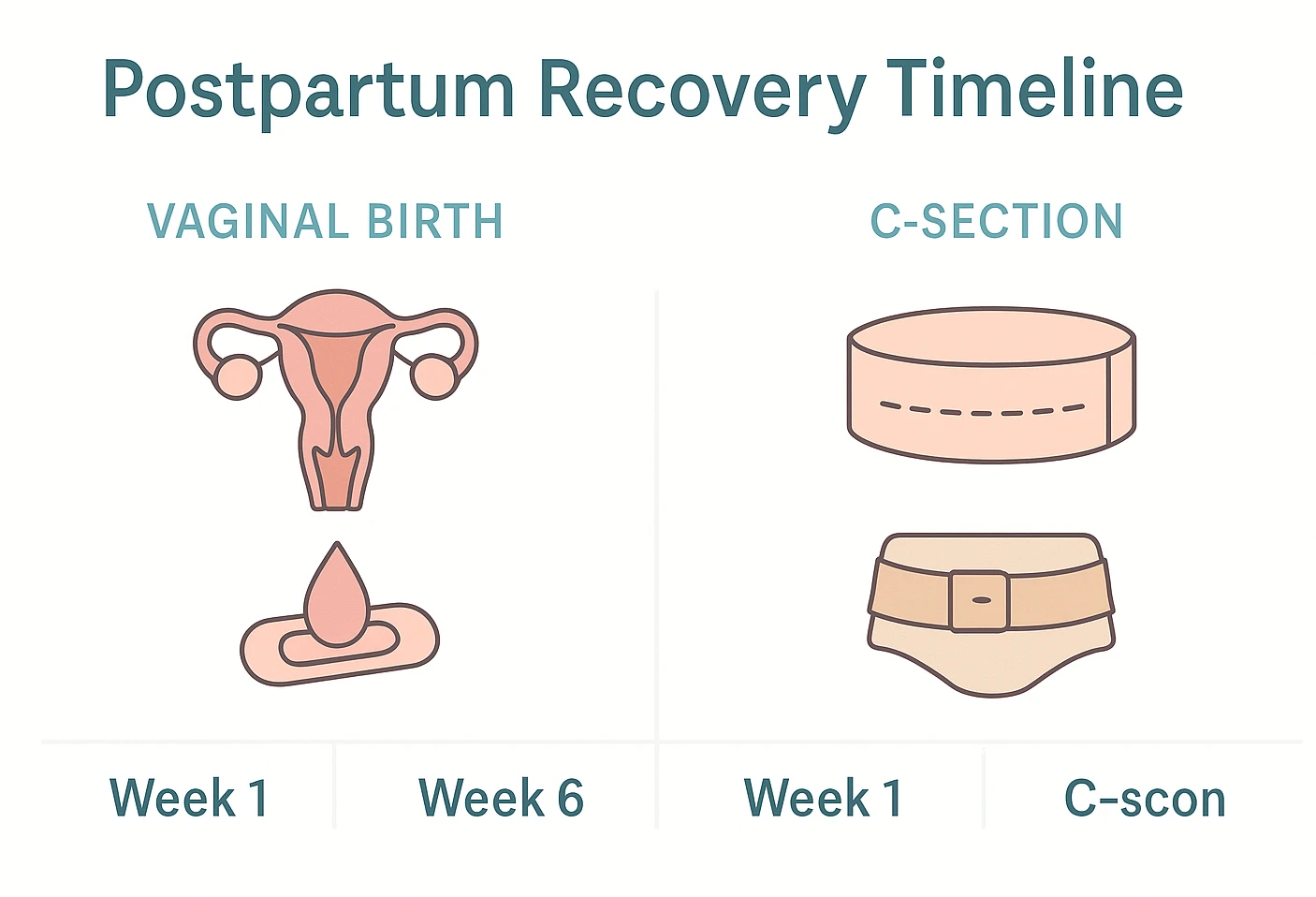
Vaginal Birth: When Is Intercourse Safe?
After a vaginal delivery, your body needs time to recover to support intimacy after childbirth. Several areas must heal before you consider resuming sex after childbirth:
- Perineum: The area between your vagina and anus may be swollen, bruised, or stitched from tears or an episiotomy. Healing prevents pain and infection.
- Timeline: Stitches typically dissolve in 1–3 weeks, but full tissue recovery may take 4–6 weeks or longer, depending on individual healing. Consult a healthcare provider for guidance.
- Vagina and Uterus: The vagina stretches during birth and gradually returns to its usual size. The uterus undergoes involution, shrinking back.
- Timeline: The uterus often returns toward its usual size by about 6 weeks—your clinician’s clearance matters before intercourse.
- Lochia: Postpartum bleeding and discharge occur as the uterus sheds its lining. Intercourse during lochia increases infection risk.
- Timeline: Lochia typically changes in color and lessens over several weeks; duration varies by individual.
Healthcare guidance often suggests waiting about 4–6 weeks for initial healing, but readiness varies. Always follow your own clinician’s advice and ask about contraception—ovulation can return before your first period.
C-Section Recovery: When Can You Resume Intimacy?
A C-section involves major abdominal surgery, requiring a unique recovery process. Key healing areas must mend before you consider resuming intercourse after childbirth:
- Incision Site: Both abdominal and uterine incisions need time to heal.
- Timeline: The outer incision may mend within 2–3 weeks, while internal healing continues over several more weeks.
- Internal Healing: Deeper layers need time even if the external wound looks healed.
- Pain Management: Discomfort may persist, affecting when you may feel ready for sex.
Typical Timeline for Postpartum Intimacy
Many ob-gyns recommend about 4–6 weeks before resuming sex. If you’re wondering how soon after childbirth can you have intercourse, that window covers early physical healing—but your provider’s clearance and your comfort matter most.
- The uterus and placental site need time to heal to reduce bleeding/infection risks.
- Perineal or incision sites should recover; stitches dissolve over time.
- Lochia should lessen/stop to lower infection risk.
- Energy gradually returns as sleep and routines settle.
“The 6-week mark isn’t a strict deadline for intimacy; it’s a guideline for initial physical healing. Emotional readiness is equally crucial.”
OB/GYN Advice, Hormonal Impacts, and Postpartum Sexual Health
Your 6-week postpartum check-up is essential for postpartum sexual health. Your OB/GYN will assess healing, discuss contraception options like IUDs or pills, and help guide your return to intimacy. Clearance doesn’t mean you’re automatically ready.
How Soon After Childbirth Can Hormones Affect Intercourse?
Hormones significantly influence your desire and comfort when considering sex after childbirth. Here’s how:
- Estrogen Drop: Post-delivery, estrogen levels may fall—especially during breastfeeding—contributing to dryness and lower libido.
- Prolactin: Breastfeeding increases prolactin, which suppresses estrogen and can amplify dryness.
- Oxytocin: Bonding hormone released during feeds doesn’t always translate to sexual desire.
Dryness and low desire are common and temporary for many. Lubricants, extended foreplay, and a clinician’s advice (including safe vaginal moisturizers/estrogen if appropriate) may help. Ask about contraception—ovulation can return before your first period.
Additionally, fatigue, body image changes, and shifting priorities can dampen interest when thinking about sex after birth. Sleep deprivation is a major libido killer. 😴 Be patient with yourself.
Managing Discomfort and Emotional Readiness
If you’re wondering when you can resume sex after childbirth, comfort matters just as much as timing. Even after clearance, discomfort or lack of desire is normal when addressing postpartum sexual well-being. Prioritizing your sexual well-being postpartum requires both physical and emotional preparation.

Physical Comfort Tips for Intimacy After Childbirth
To ease physical discomfort when returning to sex after childbirth:
- Use Lubrication: Water-based or silicone-based lubricants are ideal; avoid oil-based with condoms.
- Pelvic Floor Recovery: Childbirth can weaken pelvic floor muscles. Try:
- Kegel Exercises: Squeeze muscles used to stop urine flow for 5 seconds, relax for 5, repeat 10–15 times, 3 times daily. Explore pelvic floor exercises to strengthen muscles.
- Pelvic Floor Physiotherapy: Specialists assess muscles and provide tailored exercises. Learn more from ACOG.
- Comfortable Positions: Try woman-on-top, spooning, or side-by-side to reduce pressure on sensitive areas.
- Go Slow: Start with gentle foreplay, communicate if pain occurs, and stop if needed.
- Warm Bath: Relax muscles before intimacy with a warm bath.
Emotional Readiness for Intimacy
It’s normal to experience:
- Fatigue: Newborn care can be tiring, and rest is key.
- Self-Consciousness: Postpartum body changes are natural, and self-care can help.
- Touched Out: Constant baby contact may reduce desire for touch, which is okay.
To cope, prioritize rest, practice self-care, and acknowledge your body’s achievements. Explore self-love practices to boost confidence. If sadness or anxiety persists, consult your doctor about postpartum depression.
Communicating with Your Partner
Open communication is vital for rebuilding intimacy after childbirth and navigating when you’re ready to resume sex. Share your feelings to build understanding.
Starting the Intimacy Conversation
Pick a calm moment to share feelings—maybe, ‘I’m nervous about when it’s okay to have sex after childbirth.’ That invites care, not pressure.
Redefining Intimacy Beyond Intercourse
Focus on non-penetrative connection to ease back into postpartum intimacy:
- Cuddling, kissing, or massages.
- Shared activities like watching a movie. Try bonding exercises for couples to strengthen your connection.
- Verbal affirmations of love and attraction.
| Do’s ✅ | Don’ts ❌ |
|---|---|
| Talk openly and honestly. | Assume your partner knows your feelings. |
| Express needs and boundaries. | Feel pressured or pressure your partner. |
| Explore non-intercourse intimacy. | Ignore the topic completely. |
When to Seek Professional Support
Persistent pain or emotional challenges may benefit from professional support when addressing postpartum sexual health concerns. Consult your healthcare provider for tailored advice.
- Painful Intercourse: Could indicate scar tissue or hormonal issues.
- Severe Dryness: Beyond over-the-counter lubricants.
- Pelvic Floor Dysfunction: Symptoms like incontinence or pelvic heaviness.
- Postpartum Depression/Anxiety: Persistent sadness or worry.
Consult your OB/GYN, a pelvic floor physiotherapist, or a therapist for tailored care. Consider wellness coaching for holistic emotional support.
Intimacy Readiness Checker
No answers are saved or sent—everything stays on your device.
Are You Ready for Postpartum Intimacy?
Answer a few questions to gauge your physical and emotional readiness for postpartum intimacy and sexual well-being.
Always consult your healthcare provider for personalized advice.
Frequently Asked Questions About Postpartum Intimacy
Conclusion
Your postpartum intimacy journey is unique. Be patient, listen to your body, and seek support when needed. With time, communication, and care, you can reconnect joyfully with your partner.