
Feeling different after childbirth? Intimacy evolves too, but you’re not alone. Welcoming a baby is a life-altering joy, yet it brings big physical and emotional shifts. Many new parents ask, what can you do sexually after giving birth—safely and at your own pace? It’s a sensitive topic—often unspoken—yet vital for your well-being and relationship. This guide offers medically informed advice and gentle, post-birth intimacy tips to navigate closeness with confidence. From safe timing to creative ways to reconnect, we’ll explore how to nurture your bond while honoring your body’s healing journey. For a deeper look at the foundations of healing and recovery, check out our women’s pelvic health.
See the Readiness SnapshotTable of Contents
- When Is It Safe to Resume Sexual Activity After Birth?
- What Can You Do Sexually After Giving Birth?
- Physical and Emotional Changes to Expect
- Supporting Your Partner’s Perspective
- Communication: The Heart of Postpartum Intimacy
- Pelvic Floor Therapy for Intimacy Issues
- Postpartum Intimacy Tips & Readiness Snapshot
- When to Seek Professional Help
- Frequently Asked Questions
- Embracing Your New Intimate Journey
When Is It Safe to Resume Sexual Activity After Birth?
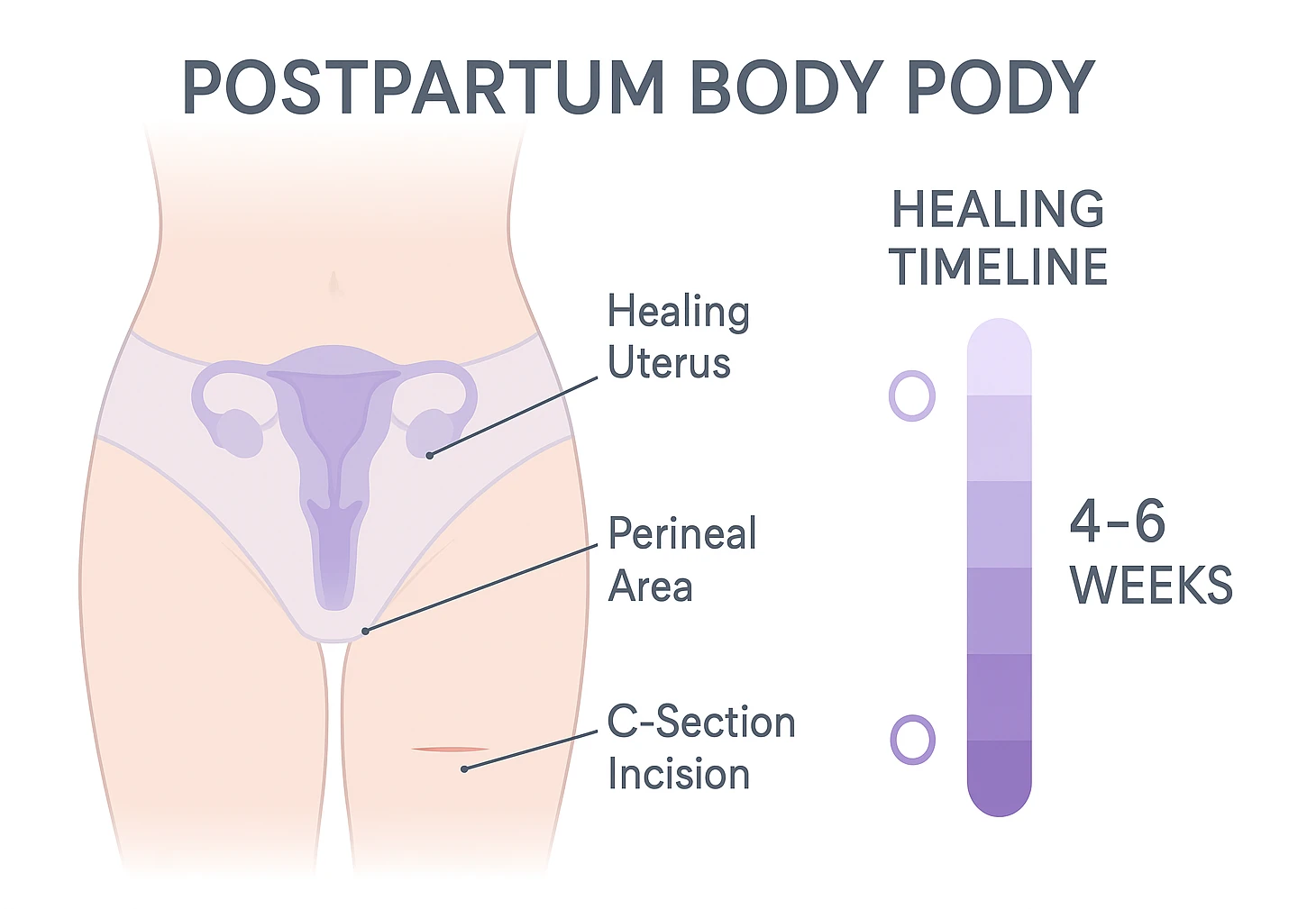
A common question is, how to safely resume intimacy after childbirth? Many clinicians recommend waiting about 4–6 weeks and/or until your postpartum check confirms healing. Every recovery is unique, so let’s break down why this timeline matters when considering your safe sexual options after birth.
Why the 4–6 Week Wait?
Your body undergoes significant healing post-delivery. For vaginal births, the perineum and uterus need time to recover. Similarly, C-sections require healing of the abdominal incision. Understanding these processes—alongside practical, post-birth intimacy tips—can clarify safe sexual options after giving birth:
- Vaginal Birth: Perineal tears or episiotomies need weeks to heal fully. The uterus shrinks (involution) and sheds lochia, which can last 4–6 weeks. Early vaginal activity may increase infection risk while the cervix is still slightly open.
- C-Section: The incision site heals externally and internally, and uterine involution still occurs. Avoid abdominal strain and vaginal activity too soon to lower complication risks.
Want a quick overview of postpartum recovery basics? See the plain-language guide at MedlinePlus.
At your postpartum check-up, your clinician can address pain, bleeding, mood, and readiness. Even if you feel eager sooner, easing in gradually helps you avoid setbacks like infection or reinjury.
This post has affiliate links. We may earn a commission. Learn more.
What Can You Do Sexually After Giving Birth?
While penetrative sex may be off-limits initially, intimacy doesn’t pause. Exploring alternative ways to connect can strengthen your bond during this transition. Here are safe ways to explore postpartum intimacy that prioritize comfort and closeness—much like these bonding exercises for couples that foster emotional connection.
Non-Penetrative Intimacy Options
Intimacy is about connection, not just intercourse. When exploring tips for postpartum intimacy, consider these gentle ways to stay close:
- Cuddling and Hugging: Touch like holding hands or snuggling releases oxytocin, fostering bonding.
- Kissing: Tender or playful kisses express affection without pelvic strain.
- Massage: A shoulder or foot massage relaxes and reconnects you with your body. Some couples make this their nightly “intimate moment.”
- Oral Sex (for the birthing parent): May be considered after lochia stops and there’s no pain or stitches—ideally after your clinician’s okay. Prioritize comfort and hygiene.
- Manual Stimulation: Gentle hand exploration allows control over pressure and pace.
- Shared Moments: Emotional intimacy—laughing together or sharing baby duties—builds a foundation for physical closeness.
Tips for Resuming Intercourse Safely
Once medically cleared and emotionally ready, ease into penetrative sex with care. These tips for postpartum intimacy help you return to intercourse comfortably:
- Go Slow: Start with gentle movements and ample foreplay to relax.
- Use Lubrication: Breastfeeding is associated with lower estrogen, which can contribute to vaginal dryness—so a water-based lubricant often helps.
- Try Comfortable Positions: Woman-on-top, spooning, or side-lying reduce pressure on healing areas.
- Communicate Constantly: Ask, “Does this feel okay?” or “Should we adjust?”
- Stop if it’s painful: Pain is your cue to pause and reassess—then check in with your clinician if it continues.
- Consider Contraception: Ovulation can return before your period—discuss birth control at your check-up.
Physical and Emotional Changes to Expect
Your body and mind transform post-birth, and understanding these changes helps manage expectations about reconnecting intimately. Let’s explore what shifts to anticipate—similar to challenges discussed in intimacy after mastectomy.

Physical Changes After Delivery
Your body may feel unfamiliar, and that’s normal. Knowing these changes—plus gentle postpartum exercises—can make intimacy feel safer as you heal. Common changes include:
- Vaginal Dryness: Lower estrogen (often with breastfeeding) can contribute to dryness. Try generous lubricant, and ask your clinician about other options if needed.
- Perineal or Incision Pain: Stitches or C-section scars may be tender for weeks. Scar tissue can also affect comfort.
- Uterine Sensitivity: Cramping—especially during breastfeeding or orgasm—is common as the uterus shrinks.
- Breast Changes: Engorged or leaking breasts during intimacy are normal if breastfeeding.
- Fatigue: Newborn care is exhausting, impacting energy for intimacy.
Hormonal Shifts and Libido
Hormonal drops in estrogen and progesterone, plus elevated prolactin (if breastfeeding), can lower libido and contribute to dryness for some people. These shifts are common and usually temporary.
Emotional and Mental Readiness
Emotional hurdles can affect intimacy as much as physical ones. You might face body image worries, a baby-first mindset, mood shifts, or fear of pain. Seek help if sadness or anxiety persists, as outlined in our guide to postpartum mental health.
Supporting Your Partner’s Perspective
The non-birthing partner also navigates changes. They may feel unsure how to approach intimacy or worried about causing pain. Encourage them to:
- Listen without judgment to your needs and fears, using tips for communicating needs in a relationship.
- Share baby care to reduce your fatigue, boosting intimacy potential.
- Express their own feelings—like feeling disconnected—to foster mutual understanding.
This two-way support strengthens your bond during recovery.
Communication: The Heart of Postpartum Intimacy
Open dialogue is crucial for navigating postpartum sexual connection. Your partner can’t guess your needs, so honest talks build trust—much like intimacy exercises for couples that deepen connection.
- Share Feelings: Discuss physical comfort, emotional readiness, and fears to align expectations.
- Reduce Pressure: Explaining fatigue or pain helps partners avoid feeling rejected.
- Use “I” Statements: Say, “I’m still healing, so I need gentle touch,” instead of “You’re pushing too hard.”
- Plan Together: Agree on what feels good, like cuddling or date nights at home.
Pelvic Floor Therapy for Intimacy Issues
Pelvic floor dysfunction—like tightness or weakness—can contribute to pain during sex. Pelvic floor therapy may help with muscle coordination, relaxation, or strength through postpartum exercises, manual therapy, or biofeedback. For example, pelvic floor exercises for post-pregnancy recovery can support healing, as noted by Women’s Health. Ask your clinician for a referral if pain continues.
Exercises After Childbirth: Gentle Starts
Exercises after childbirth like diaphragmatic breathing, light pelvic floor squeezes (without clenching), and progressive relaxation can help you rebuild comfort without strain. Start with 3–5 minutes, notice how your body feels, and increase slowly. If anything hurts, pause and ask your clinician for guidance.
- Begin with breath: Diaphragmatic breathing can down-train tension.
- Micro-engagements: Try soft “lift and let go” pulses rather than strong holds.
- Mobility first: Gentle hip circles and stretches can prepare tissues for intimacy.
Postpartum Intimacy Tips & Readiness Snapshot
Gentle 3-Step Self-Check
Educational guide only—not medical clearance. Always follow your clinician’s advice and pause if anything hurts.
Quick Readiness Checklist
Stop & call your clinician if: heavy bleeding returns, there’s a foul odor, fever/chills develop, incisions look red or drain pus, or sharp pain occurs with touch.
Proceed gently if: you’ve been cleared at your postpartum visit, have no active pain or bleeding, and feel emotionally ready. Use plenty of lubricant and choose comfortable positions.
Comfort Boosters
| Tip | Why it helps |
|---|---|
| Water-based lubricant | Offsets dryness linked with lower estrogen while breastfeeding. |
| Spooning or side-lying | Reduces pressure on the perineum or abdomen. |
| Short sessions + check-ins | Lets you adjust before discomfort builds. |
When to Get Help
| Symptom | Next step |
|---|---|
| Persistent pain with touch or penetration | Ask for a pelvic health PT referral. |
| Heavy/odorous bleeding, fever, incision redness | Contact your clinician same day. |
| Low desire or anxiety that lasts | Discuss screening and support options. |
Try This Conversation Opener
“I want closeness, but I’m still healing. Can we try cuddling and check in after five minutes about comfort?”
When to Seek Professional Help
Childbirth changes a lot, and sometimes you’ll need your clinician’s help to decide what’s safe for intimacy right now. Make that call if you notice:
- Persistent Pain During Sex: Postpartum exercises may help, but a pelvic health clinician can tailor care.
- Heavy or Foul-Smelling Lochia: Heavy bleeding that returns or smells off could signal infection.
- Infection Signs: Fever, chills, or redness/pus around stitches or incisions are red flags.
- Severe Dryness: If lube isn’t enough, ask your clinician about additional options—especially if you’re breastfeeding.
- Postpartum Depression/Anxiety: Feeling down or anxious for over two weeks isn’t just “baby blues.” Reach out to a professional for help, as explored in our postpartum mental health guide.
- Relationship Strain: Couples counseling can help you reconnect.

Frequently Asked Questions About Postpartum Intimacy
Embracing Your New Intimate Journey
Postpartum intimacy is a unique path, shaped by healing and new parenthood. By prioritizing recovery, communicating openly, and experimenting with gentle ways to connect, you can nurture your bond with confidence. If challenges arise, your clinician and pelvic health team can help you find what works.
Educational content only—not medical advice. Everyone heals differently, especially with pregnancy-related or surgical factors. Always follow your clinician’s guidance and stop any activity that causes pain.