
Pelvic floor exercises for post pregnancy can help you rebuild strength, regain confidence, and restore core stability after childbirth. Noticing bladder leaks or a sense of pelvic heaviness? You’re not alone, mama! Childbirth brings incredible changes, but it can also stress your pelvic floor muscles, which support your organs, control bladder and bowel function, and enhance intimacy. This guide walks you through gentle, effective routines tailored for new moms, so you can start your recovery journey today. For a full-body, long-term approach to pelvic recovery, explore women’s pelvic health.
Key takeaway: Small, consistent steps add up—listen to your body and go at your pace.
Note: Exercise responses vary. Research supports pelvic floor muscle training for many postpartum women, but results depend on consistency and individual factors. Always follow your clinician’s advice.
Your Postpartum Pelvic Floor Recovery Guide
Use this interactive tool to get gentle, stage-specific suggestions. Pick a phase to see safe postpartum options.
Select a phase above to get started! 🛌
Always consult your doctor before starting any new exercise.
Table of Contents
- Key Takeaways for Postpartum Recovery
- Understanding Your Pelvic Floor After Childbirth
- Why Gentle Training Matters Postpartum
- When to Start (Postpartum Pelvic Floor Exercises)
- Your Postpartum Pelvic Floor Recovery Guide
- Getting Started (Beginner steps & form)
- Gentle Postpartum Exercise Ideas
- Tips for Safe, Effective Pelvic Floor Work
- Common Challenges and Solutions
- C-Section Considerations for Pelvic Floor Recovery
- FAQ
- Conclusion
Key Takeaways for Postpartum Recovery
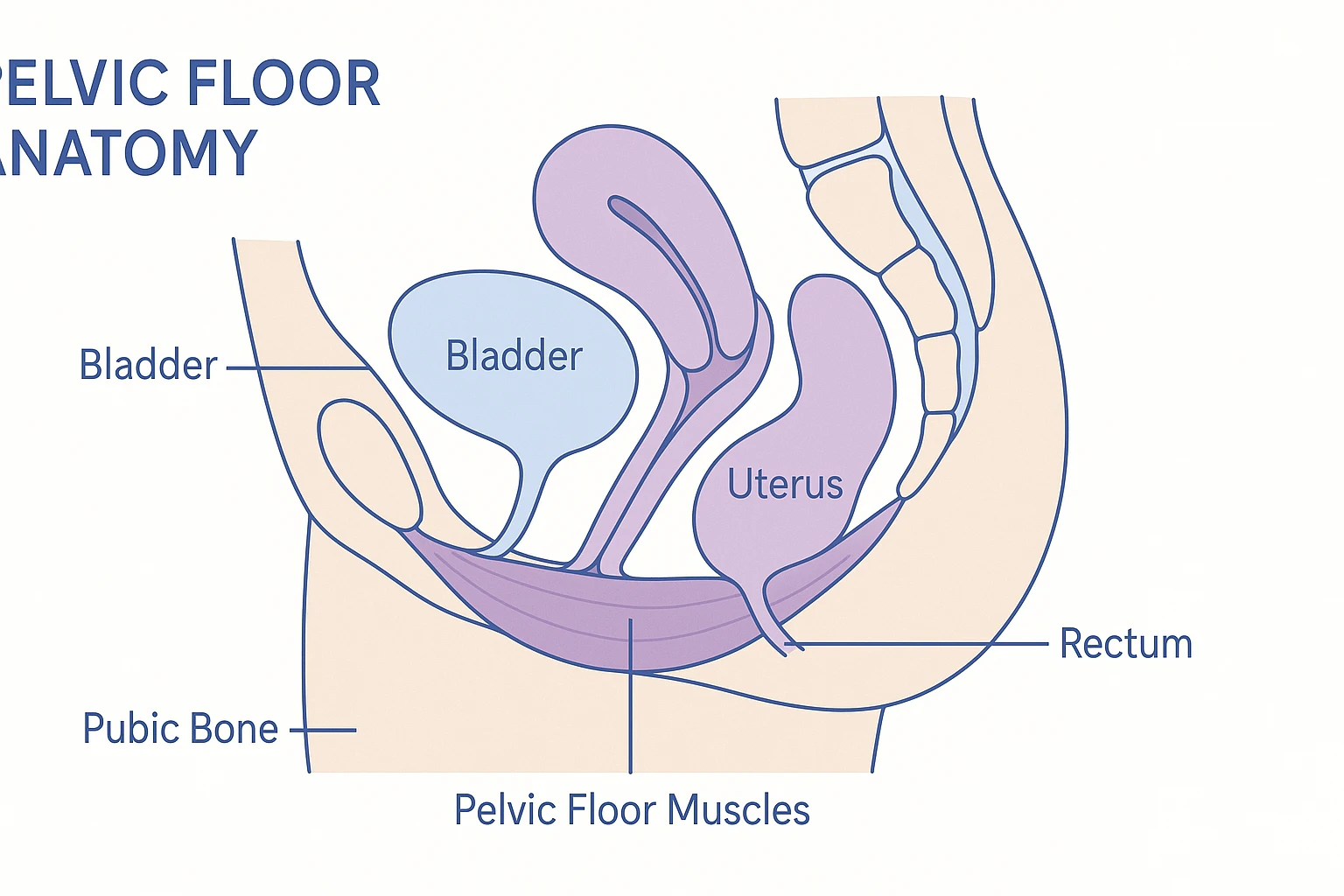
- Pelvic Floor Changes: Pregnancy and birth can stretch and weaken your pelvic floor, impacting bladder, uterus, and bowel support.
- Gentle Start: Get medical clearance before you begin. Start light and build gradually.
- Holistic Benefits: These exercises may support bladder control, reduce back pain, enhance core stability, and boost intimacy.
- Consistency Matters: Short, frequent sessions are more effective than intense ones.
- Seek Help if Needed: Persistent pain or leakage? A pelvic floor physical therapist can offer personalized support.
This post has affiliate links. We may earn a commission. Learn more.
Understanding Your Pelvic Floor After Childbirth
Picture your pelvic floor as a supportive hammock stretching from your tailbone to your pubic bone. This muscle group holds your bladder, uterus, and bowel in place, forming the foundation of your core. During pregnancy, it bears the weight of your growing baby. Then, childbirth—whether vaginal or C-section—puts it under significant strain, often requiring targeted postpartum pelvic floor training to restore strength.
How Childbirth Impacts Your Pelvic Floor
Here’s what can happen after pregnancy:
- Stretching and Weakening: Vaginal delivery stretches these muscles significantly; C-sections still involve strain from pregnancy weight.
- Nerve Impact: Pressure may temporarily affect nerves, making it harder to feel or engage your pelvic floor.
- Muscle Imbalance: Weakness can cause overcompensation elsewhere, leading to back discomfort.
- Scar Tissue: Tears or an episiotomy may create scar tissue that changes muscle function.
Many new moms notice leaking urine with coughing or sneezing (stress incontinence), pelvic heaviness, or discomfort during intimacy. Thoughtful postpartum pelvic floor work may help.
Why Postpartum Pelvic Floor Exercises Matter
Your pelvic floor muscles are unsung heroes. High-quality evidence (for example, a Cochrane Review update) shows that consistent pelvic floor muscle training can reduce postpartum urinary incontinence and improve strength. Beyond supporting bladder control, these exercises promote holistic recovery, helping you feel more confident and balanced and aiding in resuming intimacy after childbirth.
Benefits of Pelvic Floor Strengthening
- Improved Bladder Control: Stronger muscles may reduce leaks during laughter or exercise.
- Enhanced Core Stability: Your pelvic floor teams up with deep core muscles to support posture.
- Prolapse Support: Strengthening may help support organs and reduce prolapse risk.
- Better Bowel Control: Can help with gas or stool leakage, a common postpartum issue.
- Improved Intimacy: Stronger, more coordinated muscles may enhance comfort.
- Circulation & Recovery: Gentle movement supports blood flow for healing and tone.
- Long-Term Health: Investing now supports function as you age.
When to Start Postpartum Pelvic Floor Exercises
Timing depends on your healing and comfort. If you practiced pelvic floor exercises during pregnancy, you might feel ready sooner—but always get your doctor’s clearance, especially after a C-section or complicated delivery. Here’s a general roadmap:
Postpartum Recovery Timeline
- Days 1–5 (Immediate Postpartum): Rest and gentle breathing. Light awareness only. After C-section, avoid abdominal strain.
- Weeks 1–6 (Early Postpartum): With clearance, try mild contractions for connection—not strength. Avoid heavy lifting or intense core work.
- Weeks 6–12 (Mid-Postpartum): Gradually increase holds and add quick flicks. Consider pelvic floor physical therapy if you notice pain or leakage.
- Beyond 3 Months: Integrate into daily movements, progressing to dynamic activities as you feel ready.
Sound familiar? Feeling unsure is common. Start small, notice what feels good, and build slowly.
Getting Started with Pelvic Floor Exercises for Post Pregnancy
Ready to start? Getting the hang of a basic Kegel contraction is your first step to rocking postpartum pelvic floor exercises. Doing them correctly supports recovery and helps you avoid strain.
Finding Your Pelvic Floor Muscles
Not sure where to start? Try these methods to locate your pelvic floor:
- Stop the Flow: Imagine halting urine mid-stream. Those muscles are your pelvic floor. Don’t practice this regularly while peeing—it can disrupt bladder function.
- Hold Back Gas: Picture preventing gas release. Feel a lift around your anus—that’s your pelvic floor.
- Lift and Squeeze: Visualize gently lifting something with your vagina, like a small berry.
What to avoid: Don’t squeeze your buttocks, thighs, or stomach, hold your breath, or push down.
Correct Kegel Technique
Once you’ve found the muscles, try this:
- Choose a Position: Lie on your back with knees bent, feet flat. Later, try sitting or standing.
- Relax: Take deep breaths to relax your stomach, buttocks, and thighs.
- Squeeze and Lift: Inhale deeply, then exhale while gently lifting your pelvic floor up and in, like sipping through a straw.
- Hold Briefly: Start with 1–2 seconds, feeling a gentle “hug.”
- Relax Fully: Let the muscles soften completely before the next squeeze.
- Repeat: Do 5–10 repetitions, focusing on quality.
Gentle Pelvic Floor Exercises for Post-Pregnancy Recovery
Let’s explore gentle options for each recovery phase. Stop if anything hurts and check in with your clinician.
Phase 1: Early Recovery (0–6 Weeks)
Focus on reconnection and awareness, especially for C-section or vaginal delivery recovery.
1. Gentle Awareness Contractions
How: Lie on your back, knees bent. Inhale, let your belly rise. Exhale, gently lift your pelvic floor like sipping through a straw. Don’t squeeze hard.
Hold: 1–2 seconds. Relax: Fully release. Reps: 5–10, 2–3 times/day.
Why: Rebuilds mind-body connection without stressing healing tissues.
2. Elevator Kegels (Level 1)
How: Imagine your pelvic floor as an elevator. Inhale to relax (ground floor). Exhale to lift to the first floor (20–30% effort). Hold briefly, then lower.
Hold: 2–3 seconds. Relax: 2–3 seconds. Reps: 5–8, 2 times/day.
Why: Promotes controlled engagement and release.
3. Breathwork with Pelvic Floor Engagement
How: Lie or sit comfortably. Inhale deeply, expanding your belly. Exhale, draw your belly button toward your spine and lift your pelvic floor.
Reps: 5–10 breaths. Why: Links breathing with core stability.

Phase 2: Building Strength (6–12+ Weeks, with Clearance)
Once you can feel your pelvic floor, build strength and endurance.
1. Standard Kegels (Holds and Quick Flicks)
Holds: Squeeze and lift your pelvic floor (about 50–70% effort) for 5 seconds, breathing normally. Relax for 5 seconds. Reps: 10.
Quick Flicks: Quickly squeeze and release your pelvic floor. Reps: 10–15.
Frequency: 3 sets of each, 2–3 times/day. Why: Builds endurance and quick response to help prevent leaks.
2. Bridge with Pelvic Floor Engagement
How: Lie on your back, knees bent. Exhale, lift your pelvic floor, then raise your hips, engaging glutes. Inhale to lower, relaxing your pelvic floor.
Reps: 8–12. Why: Integrates pelvic floor with core and glute strength.
3. Squats with Pelvic Floor Focus
How: Stand with feet shoulder-width apart. Inhale to squat, hips back. Exhale to stand, gently lifting your pelvic floor. Keep knees behind toes.
Reps: 8–12. Why: Supports functional movements like lifting your baby.
4. Pelvic Tilts
How: Lie on your back, knees bent. Tilt your pelvis to flatten your lower back, engaging your pelvic floor. Release to a slight arch, relaxing fully.
Reps: 10–15. Why: Enhances pelvic mobility and core connection.
Phase 3: Integration and Advanced (12+ Weeks, Pain-Free)
Make pelvic floor engagement part of daily life with these steps for sustained pelvic floor healing.
1. Functional Movements (The Knack)
How: Before coughing, sneezing, or lifting your baby, gently lift your pelvic floor. Relax after. Why: Helps protect against leaks during sudden movements.
2. Walking with Pelvic Floor Awareness
How: As you walk, lightly activate your pelvic floor every few steps, keeping your posture tall. Why: Strengthens for everyday tasks.
3. Progressive Resistance (Guided)
How: Work with a therapist to try vaginal weights for a bit more challenge. Why: Adds gradual load to support long-term pelvic recovery.
4. Yoga Integration
How: Add gentle poses like Child’s Pose or Cat-Cow, engaging your pelvic floor on exhales. Reps: 5–10 cycles. Why: Encourages flexibility and strength.
| Exercise Phase | Focus | Key Actions | Reps/Frequency |
|---|---|---|---|
| Phase 1: Early Recovery (0–6 weeks) | Awareness, Gentle Reconnection | Gentle Awareness, Elevator (Level 1), Breathwork | 5–10 reps, 2–3x/day |
| Phase 2: Building Strength (6–12+ weeks) | Strength, Endurance, Coordination | Standard Kegels, Bridge, Squats, Pelvic Tilts | 8–15 reps, 2–3 sets, 2–3x/day |
| Phase 3: Integration & Advanced (12+ weeks) | Functional Strength, Long-term Health | The Knack, Walking Awareness, Yoga, (Weighted under guidance) | Ongoing, daily |
Tips for Safe and Effective Pelvic Floor Exercises
To get the most from your routine, follow these tips:
- Listen to Your Body: Stop immediately if you feel pain. Recovery is unique for everyone.
- Get Clearance: Confirm with your doctor at your 6-week check-up, especially after a C-section.
- Prioritize Consistency: Short, frequent sessions (5–10 minutes, 2–3 times/day) beat intense workouts.
- Breathe Properly: Exhale during the squeeze; inhale to relax—avoid breath-holding.
- Avoid Straining: Never push down; focus on lifting up.
- Stay Hydrated: Hydration and fiber help prevent constipation, easing strain.
- Seek a Therapist: Persistent issues? A pelvic floor therapist or pelvic floor massage tools can tailor your plan.
- Be Patient: Recovery takes months. Celebrate small wins!
- Make It Routine: Do Kegels while feeding your baby or at traffic lights for consistency.
Common Challenges and Solutions
Struggling to stay consistent? Here’s how to overcome common hurdles and keep your pelvic recovery on track:
- “I Can’t Feel My Muscles!” Try lying down and using “stop the flow” imagery. A therapist can use biofeedback for guidance.
- “I Keep Forgetting.” Link exercises to daily tasks (for example, five Kegels per feeding). Set phone reminders.
- “It Hurts.” Stop immediately. Pain may indicate scar tissue or spasms. Consult a therapist promptly.
- “I Feel Worse.” Check your technique—avoid pushing down. Worsening symptoms need professional evaluation.
- “Results Are Slow.” Track progress in a journal and celebrate small improvements, like fewer leaks.
C-Section Considerations for Pelvic Floor Recovery
While vaginal delivery often stretches the pelvic floor more, C-section moms still face challenges due to pregnancy weight and surgical recovery. Take extra care:
- Protect Your Incision: Avoid abdominal strain in the first 6–8 weeks. Focus on gentle breathing and light awareness.
- Monitor Scar Tissue: Scar tissue may affect core stability. A therapist can assess and guide you.
- Progress Slowly: Once cleared, follow the same phases, prioritizing comfort and avoiding heavy lifting.
Frequently Asked Questions
Conclusion: Rebuild Your Strength with Confidence
Your postpartum journey is a testament to your resilience, and thoughtful pelvic floor work is a powerful way to support recovery. Whether you’re tackling leaks, rebuilding core stability, or planning for long-term results with steady practice, every gentle squeeze brings you closer to a stronger, more confident you. Curious about postpartum intimacy? Explore safe ways to reconnect with your partner. Stay patient, keep at it, and don’t hesitate to see a pelvic floor therapist for tailored support. You’ve got this.
