
Women’s pelvic health is often hushed, even though it shapes daily comfort, intimacy, and quality of life. This guide explains the pelvic floor, common symptoms, and caring routines at every life stage—so you can move, love, and live with confidence. Whether you’re pregnant, noticing new symptoms, or being proactive, you’re in the right place.
30-Second Pelvic Self-Check
Answer three quick questions to see if it may be worth speaking with a clinician.
Educational tool only—this is not medical advice, diagnosis, or treatment. If you have severe pain, fever, heavy bleeding, or sudden changes, seek medical care.
Table of Contents
- Key Takeaways for Women’s Pelvic Health
- Understanding Women’s Pelvic Health: The Basics
- Common Pelvic Floor Conditions in Women
- Pelvic Health Across Life Stages
- Diagnosis & Testing
- Treatment Options for the Pelvic Floor
- Prevention Tips for Lasting Pelvic Wellness
- What’s Next in Pelvic Care
- Frequently Asked Questions
- About This Guide (E-E-A-T)
- Conclusion: Empower Your Pelvic Wellness
Key Takeaways for Women’s Pelvic Health
- Daily comfort: A responsive pelvic floor helps you move freely and reduces leaks and pain.
- Sexual well-being: Pelvic health supports comfortable, fulfilling intimacy.
- Aging with confidence: Consistent care can lower risks of prolapse and incontinence and support independence.
- Early action: Checking symptoms sooner can guide you toward simple steps and professional support when needed.
Understanding Women’s Pelvic Health: The Basics
This guide to women’s pelvic health covers the pelvic floor, common symptoms, and simple routines you can start today. New to this? Try the pelvic floor exercises for beginners women’s guide.
This post has affiliate links. We may earn a commission. Learn more.
What is the Pelvic Floor?
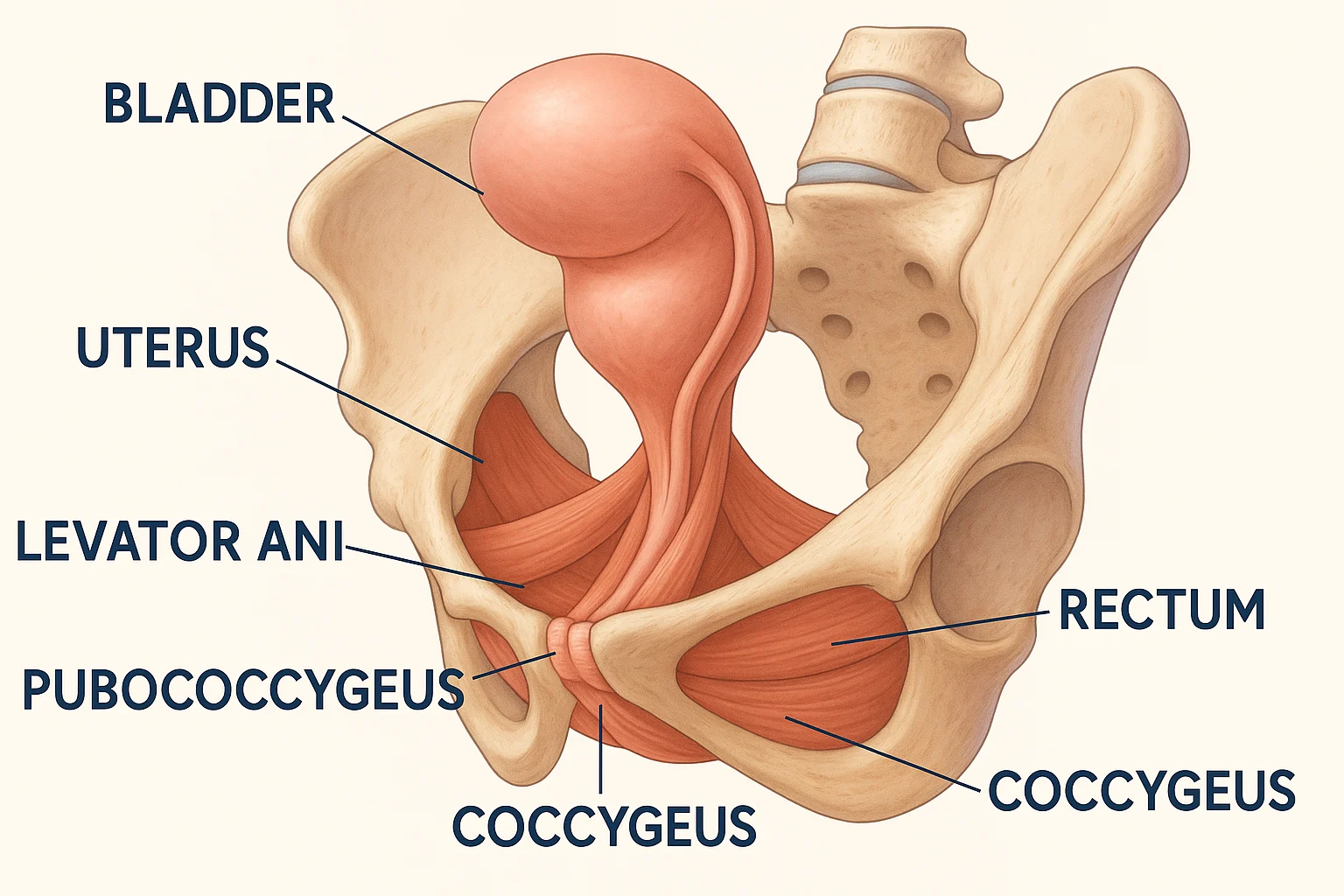
The pelvic floor is a group of muscles and connective tissues spanning from pubic bone to tailbone and sit bone to sit bone. Working with your abs, back, and diaphragm, it forms your core’s base. Strong, well-coordinated muscles support organs and continence and help posture.
Functions include:
- Support: Holds up bladder, uterus, and rectum.
- Continence: Helps control bladder and bowel function.
- Sexual function: Contributes to comfort and sensation.
- Stability: Assists spine and pelvic alignment.
- Circulation: Aids blood and lymph flow.
These voluntary muscles can be trained—just like any other—to improve control and strength. Explore pelvic floor massage techniques for added support.
Myths and Facts
Kegels aren’t a cure-all; if muscles are too tight, more squeezing can worsen symptoms. Athletes can have pelvic issues too. Your pelvic floor is unique, and strategies like reverse Kegels or biofeedback may help when tailored to you.
Common Pelvic Floor Conditions in Women
Pelvic symptoms can feel isolating, but many are treatable. For specifics, see can pelvic floor therapy help with endometriosis.
Urinary Incontinence
Accidental urine leaks are common after childbirth, with menopause, or due to high-impact activity. Therapy and lifestyle changes may help. Types include stress, urge/overactive bladder, and mixed incontinence.
Fecal Incontinence
Leakage of gas or stool can follow childbirth or surgery; constipation and nerve issues add risk. Pelvic-floor exercises may reduce discomfort.
Pelvic Organ Prolapse (POP)
When organs drop due to weak support, you may feel heaviness or a bulge. Types include cystocele, rectocele, uterine, and vault prolapse. See sexuality after hysterectomy for recovery tips.
Pelvic Pain
Persistent pain can relate to tight muscles, endometriosis, or nerve irritation. Therapy and mindful pacing may help. Common causes include dyspareunia, interstitial cystitis, pudendal neuralgia, and vulvodynia.

Overactive vs. Underactive Floor
Overactive (tight) muscles can cause pain or constipation; underactive (weak) muscles can lead to leaks or prolapse. Different issues need different plans—strengthen, relax, or both. If you’re unsure which applies, a quick screen with a pelvic floor PT can clarify the next step.
Pelvic Health Across Life Stages

Your body changes across life stages. A few key shifts—and how to care for yourself:
Puberty & Early Adulthood
Learn healthy bathroom habits, manage pain conditions early, and avoid overtraining. Gentle core-pelvic work supports lifelong wellness. Try intimacy building exercises women couples to build confidence.
Pregnancy & Postpartum
Pregnancy increases pressure on the floor; birth can stretch tissues. Postpartum exercises aid recovery. See how to do pelvic floor exercises during pregnancy and pelvic floor exercises for post pregnancy. Many new parents find that short, frequent sessions fit better than long workouts.
Perimenopause, Menopause & Beyond
Hormonal shifts can influence tissue elasticity and continence. Many people benefit from pelvic floor exercises, moisturizers, and—when appropriate—hormone therapy, guided by a clinician. If dryness or urgency creeps up, a short chat with your clinician can save months of frustration.
Diagnosis & Testing
If leaks, heaviness, or pain persist, check in with a clinician. You can also explore how to use a pelvic floor massage tool to discuss at your appointment.
Common Tests Explained
Pelvic ultrasound: A probe on the lower belly or in the vagina uses sound waves to create images of the bladder, uterus, and surrounding tissues. You may feel pressure but it shouldn’t be painful. Results can show organ position, thickness, or cysts—helping rule in or out causes like prolapse or uterine changes.
Urodynamic testing: Measures how the bladder stores and releases urine. Small catheters track pressure and flow while you slowly fill and empty the bladder. It can feel odd but is usually brief. Findings help differentiate stress vs. urge incontinence so treatment plans match what’s really happening.
Exam and screening: A gentle pelvic exam checks muscle tone (too tight, too weak, or mixed), reflexes, and areas of tenderness. Your clinician may recommend a stool or urine test, or refer to a pelvic floor physical therapist for a movement-based assessment. Bring a short symptom log—what triggers leaks or pain—to speed up the plan.
Comfort tips: wear easy clothes, arrive with questions written down, and ask for pauses during any exam. You’re in charge of the pace.
Treatment Options for Pelvic Floor Health

Many treatments help—from conservative care to medical options. Consider a device for pelvic floor exercise if recommended by your clinician.
Pelvic Floor Physical Therapy (PFPT)
PFPT can be tailored to weak or tight muscles and may improve confidence and control. Common techniques:
| Technique | Purpose | Best For |
|---|---|---|
| Kegels | Strengthen pelvic floor | Incontinence, prolapse |
| Reverse Kegels | Relax tight muscles | Pelvic pain, constipation |
| Biofeedback | Improve muscle control | Weak or overactive muscles |
| Manual Therapy | Release muscle tension | Pain, tightness |
Quick-Start Exercises (pick the pattern that fits)
If you suspect an overactive (tight) floor:
- Diaphragmatic breath (60 seconds): One hand on ribs, one on belly. Inhale through the nose and imagine the pelvic floor “melting” down and wide; exhale gently, no squeeze.
- Hip drop + sigh (30–60 seconds): Seated, let one hip soften toward the chair while you sigh out; switch sides. Keep shoulders loose.
- Reverse Kegel cue (30–60 seconds): Picture “releasing a pebble” or “opening a flower.” No pushing or bearing down.
Goal: Decrease guarding, ease pain with exams or intimacy, and improve coordination. Stop if pain increases; a PT can tailor positions and pacing.
If you suspect an underactive (weak) floor:
- Foundational Kegels (60–90 seconds): Exhale and gently lift as if stopping urine or gas; inhale and fully let go. Aim for smooth lifts, not maximal squeezes.
- Endurance hold (2–3 reps): Light lift for 5–8 seconds; rest twice as long. Quality over intensity.
- Functional cue (30–60 seconds): Before a cough, lift slightly; then release. Practice this “pre-brace” during daily triggers.
Goal: Support continence and reduce heaviness. If bulge or pain appears, ease off and seek guidance.
Lifestyle Changes
Keep it simple: fiber + hydration, daily gentle movement, and 5 minutes of pelvic floor practice. Reduce bladder irritants if sensitive (e.g., caffeine). See the beginners guide for quick routines. If you sit long hours, set an hourly stand/walk reminder to ease pressure.
Medical Interventions
Depending on your diagnosis, options may include medications (for OAB), pessaries (for prolapse), or surgery in selected cases—guided by a specialist. Your plan should match your goals, lifestyle, and comfort level.
Emerging Treatments
Some clinics offer energy-based vaginal treatments (e.g., lasers, RF). Evidence is mixed and they aren’t FDA-approved for “vaginal rejuvenation.” Discuss risks and proven first-line options like PFPT with your clinician.
Heads-up: The FDA has cautioned against using energy-based devices for “vaginal rejuvenation.” Consider alternatives with your clinician. See professional guidance (opens in new tab). ACOG committee opinion.
Prevention Tips for Lasting Pelvic Wellness
- Maintain posture to reduce pressure.
- Avoid straining during bathroom visits.
- Use breathwork to relax muscles.
- Communicate openly with partners about intimacy challenges.
Want a handy list? Download the free pelvic health checklist to keep your women’s pelvic health routine on track. You’ll need a PDF reader like Adobe Acrobat (free at get.adobe.com/reader).
What’s Next in Pelvic Care
AI-guided trainers and better biofeedback tools may expand options, but proven basics—PFPT and mindful exercise—remain smart first steps as research evolves. Telehealth makes it easier to find a specialist and follow a plan that fits your day.
Frequently Asked Questions
About This Guide (E-E-A-T)
This educational guide summarizes widely used approaches in pelvic care and aims to support informed conversations with your clinician. We avoid “quick fixes” and don’t promise cures. Tools and exercises here are general; if you have pain, bulge, pregnancy-related concerns, recent surgery, or new symptoms, please seek personalized care from a qualified professional.
Editorial standards: we favor conservative first-line care (pelvic floor physical therapy, behavior change) and clearly label affiliate recommendations. External medical guidance is referenced where appropriate (see ACOG link above). We may update content as research evolves.
Conclusion: Empower Your Pelvic Wellness
Your pelvic wellness journey matters. Understand your body, check in early when symptoms pop up, and build steady habits—you can thrive at every stage. If today’s self-check raised questions, consider a brief consult with a pelvic floor therapist or clinician to plan your next best step.